In a September 27th letter to our employees we made a promise that we would take “a different path”, that we valued the treatment and outcomes provided, and that as a result we would continue to treat our residents based on individuals needs after October 1st.
We also said that this may sound “radical” but that it was the right thing to do.
“Radical”?
Perhaps not.
Let’s examine, for example, the potential CMS audit areas that have been noted in proposed and final rule.
Focus items are as follows:
-
Changes in payment that result from changes in the coding or classification of SNF patients vs. actual changes in case mix.
-
Changes in the volume and intensity of therapy services provided to SNF residents under PDPM compared to RUGIV.
-
Compliance with the group and concurrent therapy limit.
-
Any increases in the use of mechanically altered diet among the SNF population that may suggest that beneficiaries are being prescribed such a diet based on facility financial considerations, rather than for clinical needs
-
Any potential consequences (e.g., over-utilization) of using cognitive impairment as a payment classifier in the SLP component.
-
Facilities whose beneficiaries experience inappropriate early discharge or provision of fewer services (e.g., due to the variable per-diem adjustment).
-
Stroke and trauma patients, as well as those with chronic conditions, to identify any adverse trends from application of the variable per-diem adjustment.
-
Use of the interrupted-stay policy to identify SNFs whose residents experience frequent readmission, particularly facilities where the readmissions occur just outside the 3-day window used as part of the interrupted-stay policy.
Furthermore, CMS has clearly outlined in their updated Program Integrity Manual reviewers will be assessing for including:
-
If some skilled services were appropriate, but some services provided were not reasonable and necessary or were not supported by the medical record as having been provided as billed, and the reviewer determines (based on data entered from the medical record into the MDS QC System Software)
-
There is another case-mix classifier for which the beneficiary qualifies, the Medicare contractor shall pay the claim according to the correct case-mix classifier calculated using the MDS QC System Software for all covered days associated with that MDS, and recoup any over payments as necessary.
Broad River Rehab is pleased to report the outcomes of choosing a different path.
First, our customers have seen the benefits of capturing case mix accuracy and documentation consistency across the interdisciplinary team (IDT) via the use of the following tools:
-
Document Navigator™
-
PDPM Navigator™
-
CASPER Scanner™
-
Staffing Navigator™
Second, and more importantly, the proof of a different path is in the numbers reported below.
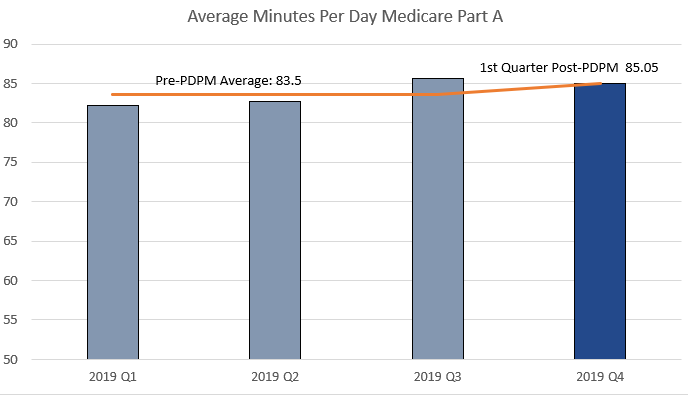
Broad River Rehab stands by our word, we support our therapists and communities alike, and as a result we continue to provide a high level of quality skilled care to our patients.
Want to learn more?
