It’s Christmas time again. Hard to believe, isn’t it? Where did 2022 go? Maybe we’re enjoying the return to some normalcy after two years of COVID realities we forgot the time.
In our haste to 2023, we should reflect on the changes to the 5- star rating in the last year. Namely, the cut point revisions that CMS intends to implement every 6 months.
In November we held a special BRR Reflections detailing the changes with some interesting graphics showing state and national changes. To access the presentation, click here. You must be a Broad River Rehab Customer with Insiders to access this exclusive content. Broad River Rehab customers can become a BRR Insider by clicking here.
What’s Happening
In March 2019, CMS released memorandum QSO-19-08-NH, outlining plans to update the quality measure (QM) rating thresholds every six months.
The plan was to increase the thresholds by 50% of the average rate of improvement in QM rating scores.
For example, if there is an average rate of improvement of 2%, the QM rating thresholds would increase by 1%. This action aims to incentivize continuous quality improvement.
Additionally, it reduces the need to have larger adjustments to the thresholds in the future.
These updates were held due to the pandemic. CMS began implementation in April 2022, and then updated again with the October 2022 refresh.
So, What Changed?
There have been two quality measure cut point updates since CMS implemented this policy: April and October. Consequently, CMS released a revised Five-Star Quality Rating System Technical Users’ Guide with the most recent QM rating thresholds with both updates.
The changes that CMS made, and will continue to make, affect the long stay, short stay and overall cut point thresholds. The individual measure cut point thresholds have not changed. Many facilities experienced quality measure 5-star rating changes simply due to the cut point changes
This was a surprise to many of us. We anticipated that that points associated with the individual measures that improved would themselves be affected, which would affect the overall cut points.
I’m Curious, are You?
When the first update happened in April, I was immediately curious as to which quality measures improved. Because CMS only revised the overall cut point thresholds it was not immediately obvious in April or October which measures showed improvement.
As we began to unpack the data, two important data facts caught my attention:
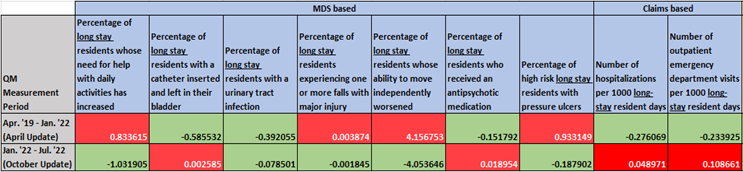
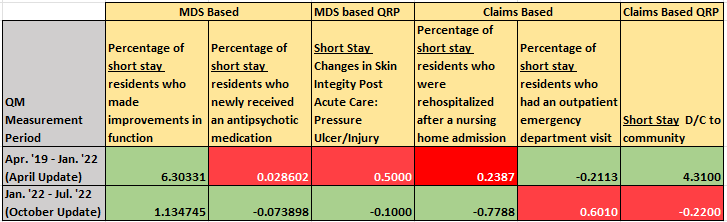
- The timeframes used to measure improvement: For the April update a 3+ year timeframe, April 2019 – January 2022 was used. For the October update a 6-month period, January 2022 – July 2022 was used.
- The measures that showed improvement that ostensibly drove the cut point changes were noteworthy. Here’s a breakdown:
In the data tables below, a green box indicates improvement, and a red box indicates decline. Do you notice anything interesting? I sure do.
What’s Interesting?
The most interesting detail that jumped out at me right away is that the improvements that drove the cut point changes in the October update to five-star, may well have been an artifact of the COVID pandemic effect on nursing homes.
In other words, during COVID, there were obvious areas of decline that would naturally improve as COVID wanes. For example, from April 2019 – January 2022, the long stay ADL related measures and pressure ulcer measure naturally declined. The improvement in these QMs that resulted from waning COVID impacted the October QM cut point update.
Also notice the short stay improvement in function doubled in its improvement between the April update and the October update, another possible artifact of COVID that affected the October update.
The QMs that improved during COVID, catheters, UTI’s, long stay antipsychotic use, and long stay hospitalizations and ED visits, are also interesting since they were the ones that affected the impacted the April update. These also may have been an artifact of COVID in terms of the kind of patients that were in SNFs during that time. It’s the UTI improvement during that time that surprised me most given the spotlight on infection control and the issues that nursing homes had with staffing during the reporting period.
On the short stay side, the usual suspects appear, and the improvement vs. decline in QMs is not surprising. Pressure ulcers, and rehospitalizations both declined relative to the April update and then improved as they impacted the October update. The interesting one to me from the short stay perspective is the short stay antipsychotic measure. The increase in new antipsychotic use over COVID is a mystery. Perhaps this was a relative increase given that fewer residents were admitted as short stay during that time period.
Final Thoughts
Whatever the cause of these changes, we have been the recipients of two updates so far. This will continue to affect SNFs ongoing. The next update to the QM cut points is in April. It will be interesting to see what that brings us. I anticipate we may see further improvements given that the COVID impact is lessening compared to the prior measurement periods.
It will also be interesting to see how CMS will adjust when the new MDS is implemented in October 2023. What will the transition to QMs without section G do to the improvements in the cut points in April 2024, particularly related to the QMs that currently rely on section G to calculate?
It is the LS Percentage of residents whose ability to move independently worsened, Long Stay Percentage of residents whose need for help with daily activities has increased and Short Stay Percentage of residents who improved in their ability to move around on their own, that are currently calculated with items coded in section G. Furthermore, the Short Stay Percentage of high-risk residents with pressure ulcers is adjusted with covariates coded in section G.
Knowing what improvements occurred nationwide from quarter to quarter is helpful, particularly as facilities with limited resources look to focus on areas on which they can have a meaningful impact.
It is important when we look at the numbers that it is the resident who is representative of what a facility 5-star rating looks like from quarter to quarter. As the new year approaches, and the January care compare updates approach, we should keep this in mind and work diligently to ensure that our quality focus is all about who we serve.
