It’s been a while since we focused on North Carolina Medicaid. There is actually a lot going on. We going to cover some of it today.
Some reference material that will be handy for this post are the current rates. You can download those here.
COVID-19 Add-On
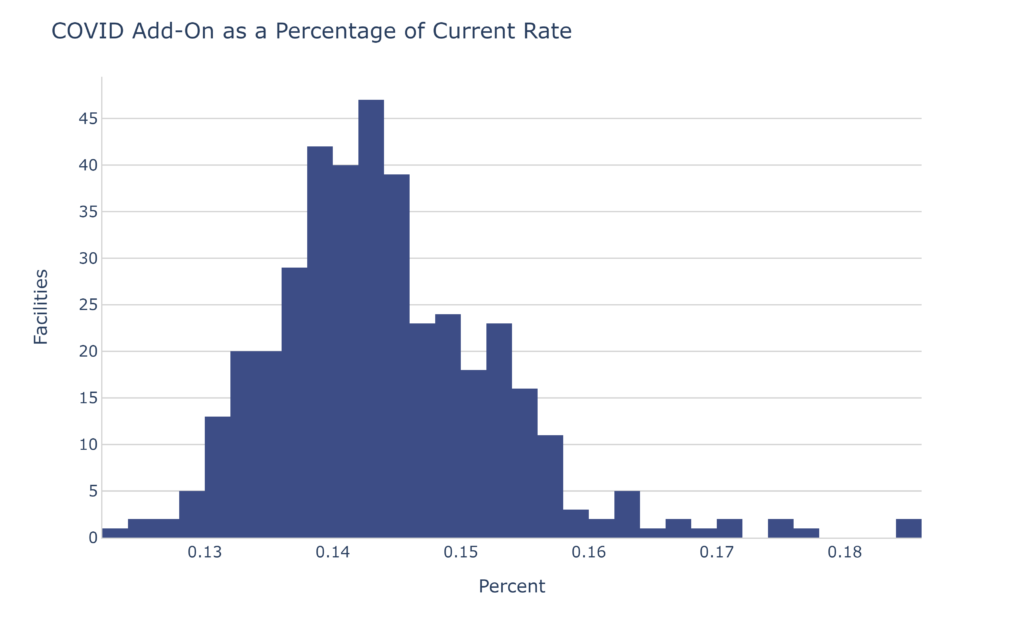
Currently all Medicaid paid days include an add-on for COVID-19 of $37.74. While the state hasn’t made an official announcement, with the end of the PHE, we should at least consider the possibility that this benefit could end. (If you’ve heard something from the state or if you are the state and would like to share some information, please contact me.)
That $37.74 represents 14.4% of the overall rate for the average facility.
If that doesn’t get your attention, let’s turn that into dollars:
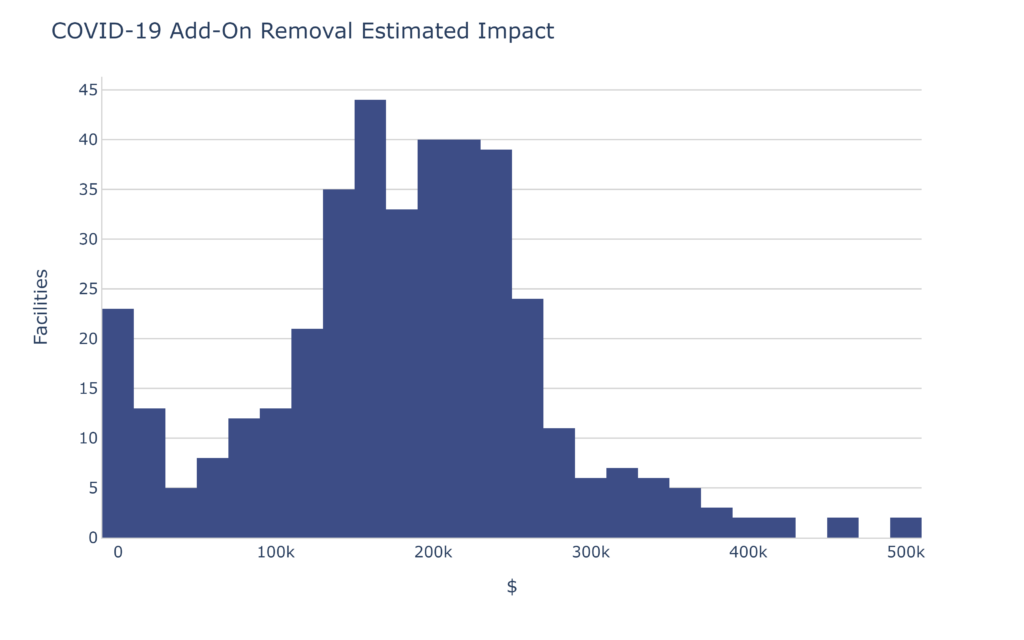
The average skilled nursing facility could see a reduction of $137,402.60 per quarter. Note that number is skewed downward by facilities that have zero Medicaid. With the non-Medicaid facilities removed, the average is $190,234.69. From the perspective of the state, this is more than $74M quarterly. You can appreciate that this would be of interest to the state.
Let me repeat, I’ve heard nothing regarding this benefit actually going away.
Rate Floors
Currently, your Medicaid rate has a floor. I’ve noticed that a lot of people I talk to are not aware of this. This means that if your facility’s calculated rate is lower than the rate from the previous quarter, the previous quarter rate remains in effect.
Currently 53.8% of skilled nursing facilities in the state are taking advantage of this. That means more than half of the state’s facilities would see a reduction in Medicaid rate if this policy were to change.
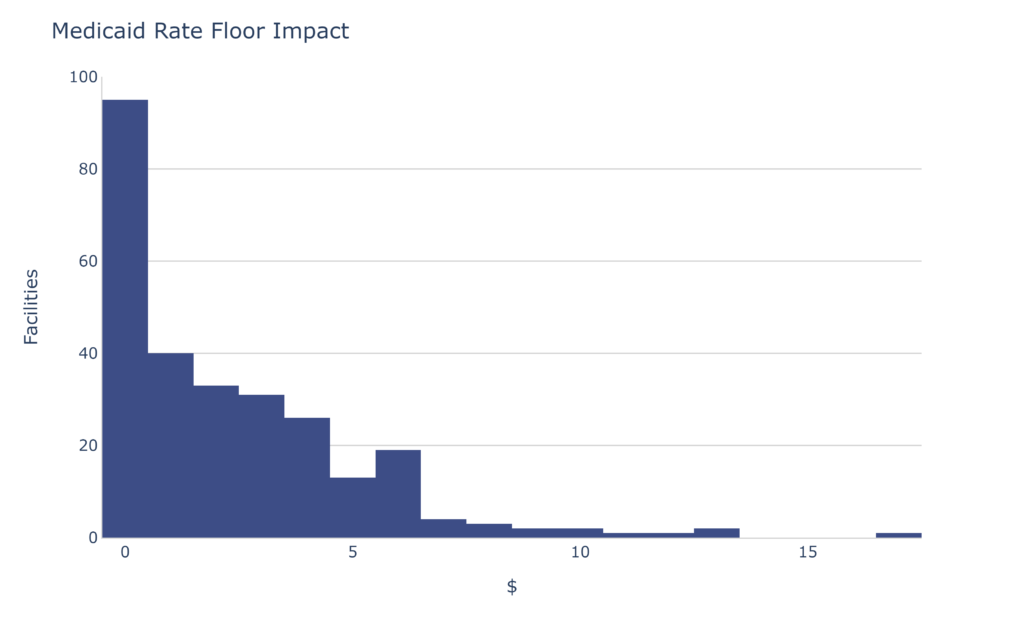
I’ve removed the zeros from the data. (There are still quite a few very near zero.) As you can see, the potential rate floor impact is modest compared to the COVID-19 add-on, however $3-$4 per Medicaid day can be a lot. The average change for those utilizing the rate floor is $2.35 PPD.
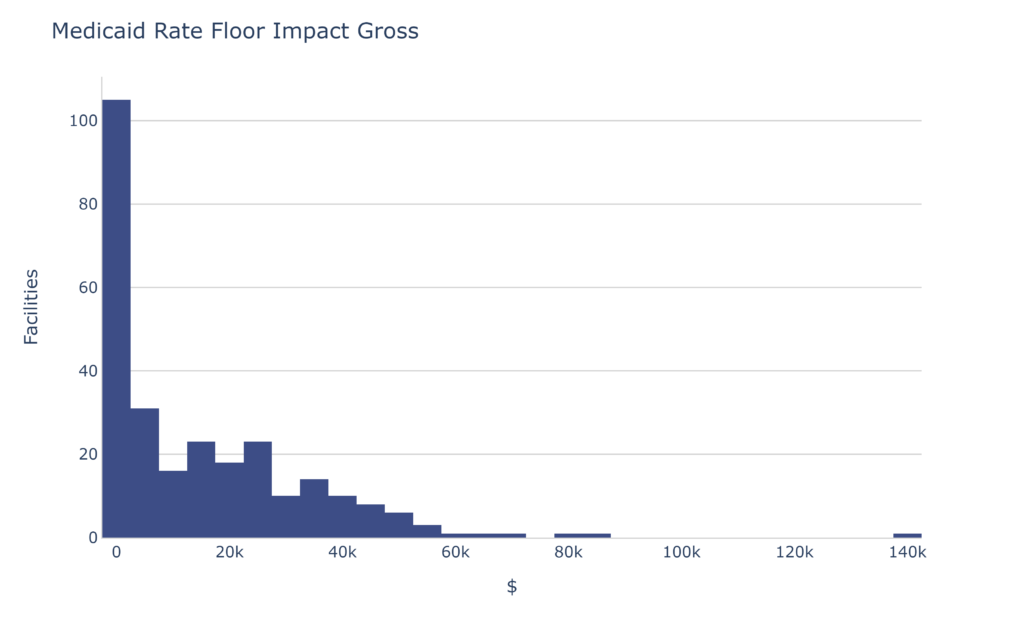
If the rate floor policy were to be discontinued, the average impact to those facilities currently utilizing it would be roughly $15k per quarter.
Assessment
This one is more complex. There is a little-discussed part of your Medicaid rate labelled “Assessment”. This part of the rate has come into focus more recently because the state has recently changed the rules a little and it now impacts more facilities. You can read the rule here. It’s not legalese, I promise.
The important part says:
NCDHHS
- The assessments imposed on nursing facilities will be calculated as follows:
- Continuing Care Retirement Centers and Tribal Facilities will be assessed at a uniform per diem rate equal to $0.00 per non-Medicare day.
- Nursing facilities with a total annual census greater than 42,000 will be assessed at uniform per diem rate equal to $8.64 per non-Medicare day.
- All other nursing facilities that do not meet the criteria of (a) or (b) above will be assessed at a uniform per diem rate equal to $26.74 per non-Medicare day.
I added the emphasis. Pay close attention to that 42,000 “annual census”. I believe that is in days and includes ALL payers.
42,000 ÷ 365 = 115
That means if you average right around 115 patients in your facility, and you aren’t a CCRC, you may experience swings of $18.10 per Medicaid day from quarter to quarter. A 125 bed facility at 90% average census would be at 112.5, dangerously close to losing $18.10 per Medicaid day.
74 facilities in the state fall into the “danger zone” of 115 to 130 beds where there likelihood is reasonable to bounce around 42,000 days per rolling year.
Self-Assessment
An easy “back of the envelope” way to check your facility is to multiply the number of beds in your facility by your typical census percentage. For example:
120 beds × 95% = 114 ← Close, but still good
130 beds × 90% = 117 ← Oops!
In that second scenario, if that 130 bed facility had 60 Medicaid residents, the Medicaid reimbursement would be $18.10 × 60 × 90 = $97,740 less than if roughly 2 few admissions had occurred over the course of a year.
Making matters more complex, if you are close to the magical 42,000 days, you probably need to weigh which payers you might be picking up. If you are working on census building and you are around the 42,000 days, you might need to cover $100k in a quarter. In that case there is a big difference between a $550/day PDPM resident, a $325 Med A replacement patient and a $263/day Medicaid resident. (BTW: $262.81 is the average Medicaid rate without the COVID add-on.)
$100k might be 2 PDPM patients for the quarter. It could also be 3.4 Med A Advantage residents or even 4 additional Medicaid residents. Remember, that’s for the entire quarter. That means you would need to average 2 additional PDPM residents over the 90 days. (or some mix)
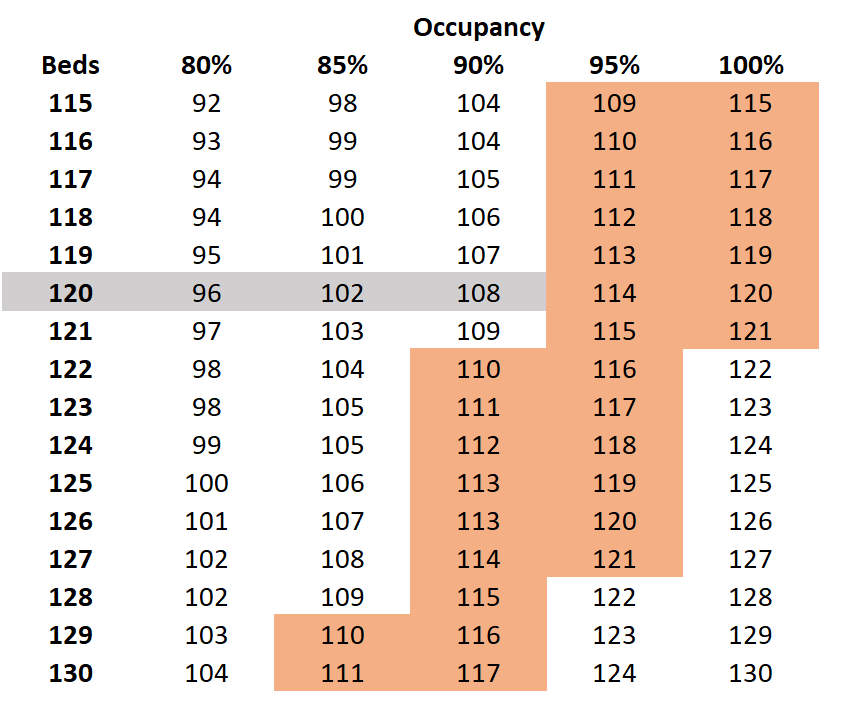
Obviously this one requires a little more expertise to get right. You need to be aware of not just your occupancy, but also your rates. Unfortunately, in looking through the data I see a few facilities are *just* above 115. There’s nothing like a lump of coal for your census development efforts.
If you want to dive deeper into your facility, contact me.
FRV
FRV stands for “Fair Rental Value” and is essentially a measure that reflects the age of your facility. You can read more about it here. The quick and easy boil-down of FRV is this “If you haven’t done capital improvements in a while, you will be paid less.” It’s a simple concept but the details of actually doing a capital improvement are complex.
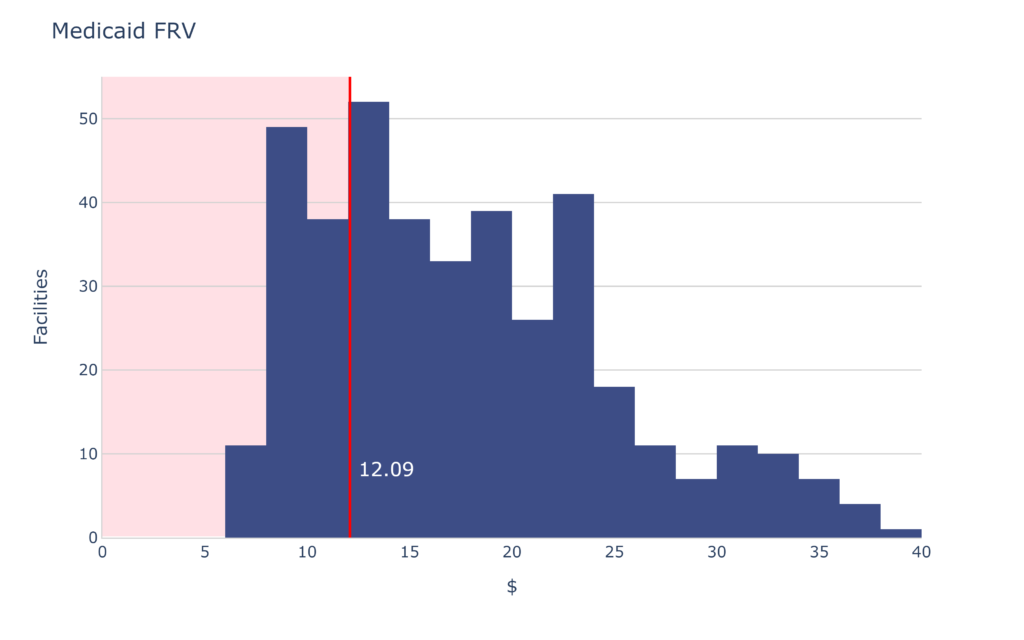
If your FRV is less than $12, you should be considering capital improvements. Consult an expert.
PDPM for Medicaid?
A few states have already made the switch to a PDPM-style Medicaid system. Most have made significant changes like dropping PT/OT, NTAs and more. (Not supported by any research that I’ve seen either.)
To date, North Carolina has not said anything officially about a move to a PDPM-style system. I think a lot of us suspect that’s on the way. The best advice is to prepare now.
That means making sure your documentation is accurate, thorough, and covers ALL the conditions that are true about the resident. You’re going to do the care. Make sure you’re compliant and get reimbursed properly. The best way to do that is artificial intelligence (AI). Broad River Rehab is actively using AI for admissions AND internal auditing. Contact us right now for a demo.
