In just a few short weeks, we will begin the second FY since the initiation of the PDPM. With the unprecedented encounter we have had with the COVID PHE, there have been decisions on the part of CMS to limit the number of obvious changes that were to take effect this fall. However, due to the regular rule making Cycle, there are still some major changes headed our way on October 1. Here we detail the major provisions of the FY 2021 Final Rule. It’s time to get ready for FY 2021.
FY 2021 Final rule posted April 10, 2020
• Contains generally only program updates related to payment and PDPM have been made.
Market Basket Update
• Every year CMS updates the PPS rate based on the overall cost of goods and services that contribute to expenditures required to run and maintain a nursing facility
• This update is further revised by forecast error and multifactor productivity adjustments
• For FY 2021, the final update to the PPS rate is +2.2%
• Accordingly, the overall economic impact of this Final rule is an estimated increase of $750 million in aggregate payments to SNFs during FY 2021.
• TABLE 16 in the Final rule indicates Impact to the SNF PPS for FY 2021.
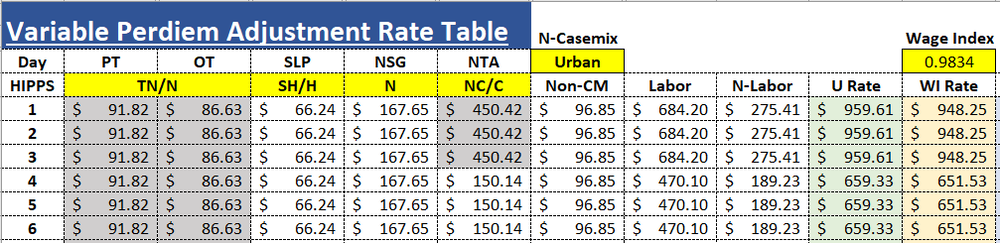
Example Rate tables Same CBSA
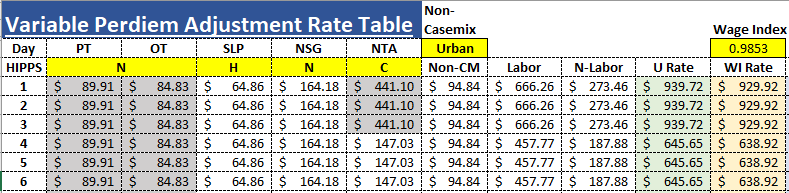
FY 2021 Final Rule Oct. 1
Wage Index Changes
• CMS has finalized adoption of the revised OMB delineations identified in OMB Bulletin No. 18-04 in order to identify a facility’s urban or rural status: OMB Memo: https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf
• CMS believes that these updated OMB delineations more accurately reflect the contemporary urban and rural nature of areas across the country, and that use of such delineations would allow them to more accurately determine the appropriate wage index and rate tables to apply under the SNF PPS, in order to enhance the accuracy of payments under the SNF PPS. Changes to the OMB statistical area delineations include some new CBSAs, urban counties that would become rural, rural counties that would become urban, and existing CBSAs that would be split apart. Tables 11-14 in the final rule include Urban counties that would become Rural, counties that would gain Urban status, CBSA’s that change name or number and Urban counties that would move to another Urban CBSA.
• CMS has finalized a 1-year transition for FY 2021 under which we would apply a 5% cap on any decrease in a SNFs wage index compared to its wage index for the prior fiscal year (FY 2020).
• Specific Wage index data may be found in the wage index tables including a table that indicates any revised Wage index data and the 5% capped wage indexes. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/WageIndex
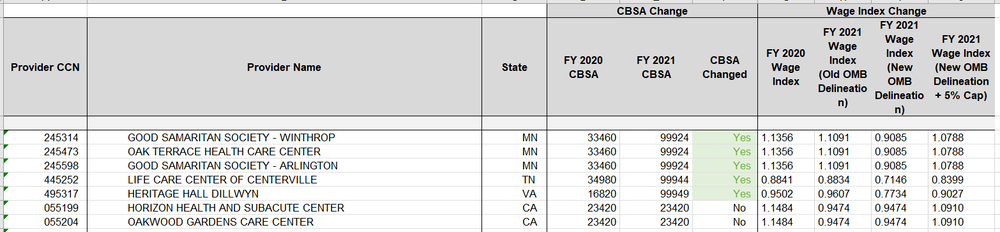
Wage Index Example
Administrative Presumption of Coverage
• Annually CMS designates those specific classifiers under the case-mix classification system that represent the required SNF level of care. This designation reflects an administrative presumption that those beneficiaries who are correctly assigned one of the designated case-mix classifiers on the initial Medicare assessment are automatically classified as meeting the SNF level of care definition up to and including the assessment reference date (ARD) of the 5-Day assessment.
• This presumption recognizes the strong likelihood that those beneficiaries who are assigned one of the designated case-mix classifiers during the immediate post-hospital period would require a covered level of care, which would be less likely for other beneficiaries.
• This administrative presumption policy does not supersede the SNF’s responsibility to ensure that its decisions relating to level of care are appropriate and timely, including a review to confirm that any services prompting the assignment of one of the designated case-mix classifiers (which, in turn, serves to trigger the administrative presumption) are themselves medically necessary.
• CMS Pub 100-2 Ch. 8 https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c08pdf.pdf
• For services furnished on or after October 1, 2019, the following are designated case-mix classifiers under the Patient Driven Payment Model (PDPM) relative to the administrative presumption of coverage:
-
Nursing groups encompassed by the Extensive Services, Special Care High, Special Care Low, and Clinically Complex nursing categories;
-
PT and OT groups TA, TB, TC, TD, TE, TF, TG, TJ, TK, TN, and TO;
-
SLP groups SC, SE, SF, SH, SI, SJ, SK, and SL; and
-
The NTA component’s uppermost (12+) comorbidity group.
ICD-10 Mapping Changes
CMS has finalized several changes to the PDPM ICD-10 code mappings and lists.
• In the current ICD-10 to clinical category mapping being used in FY 2020, ICD-10 codes associated with certain cancers that could require a major procedure do not include the option of a major procedure in the prior inpatient stay that may impact the plan of care. CMS has finalized adding surgical clinical category options of “May be Eligible for the Non-Orthopedic Surgery Category” or “May be Eligible for One of the Two Orthopedic Surgery Categories” to the clinical category mapping these diagnoses when a major procedure is identified on the MDS because a major procedure for these codes in a prior inpatient stay could affect the plan of care.
• Glucose-6-phosphate dehydrogenase (G6PD) deficiency without anemia: In the FY 2020 ICD-10 to clinical category mapping, the ICD-10 code D75.A “Glucose-6-phosphate dehydrogenase (G6PD) deficiency without anemia” is assigned to the default clinical category of “Cardiovascular and Coagulations” to align with the other D75 codes. However, G6PD deficiency without anemia is generally asymptomatic and detected by testing. Compared to other blood diseases in the D75 code family, D75.A is very minor and likely asymptomatic. For this reason, has finalized changing the assignment of D75.A to “Medical Management”
• Certain fracture codes map to the surgical default clinical categories such as “Orthopedic Surgery (Except Major Joint Replacement or Spinal Surgery)” or “Major Joint Replacement or Spinal Surgery” even if no surgery was performed. The specific codes are S32.031D, S32.19XD, S82.001D, and S82.002D through S82.002J. Because of this, CMS has finalized a change to the default clinical category associated with these codes to “Non-Surgical Orthopedic”, with the surgical option of “May be Eligible for One of the Two Orthopedic Surgery Categories”, for these codes.
• CMS has finalized a change to the default clinical category of the following fracture codes to “Return to Provider” because these codes are unspecific and lack the level of detail provided by more specific codes as to whether the condition is on the right or left side of the body: S82.009A, S82.013A, S82.016A, S82.023A, S82.026A, S82.033A, S82.036A, and S82.099A.
• In the FY 2020 ICD-10 to clinical category mapping, the M48.00 through M48.08 spinal stenosis codes have a default clinical category mapping of “Non-Surgical Orthopedic/Musculoskeletal” and no surgical option, which does not allow for coding in cases where patients have spinal stenosis and spinal laminectomy surgery. For this reason, CMS has finalized adding the surgical option of “May be Eligible for One of the Two Orthopedic Surgery Categories” to M48.00 through M48.08 spinal stenosis codes.
• In the FY 2020 ICD-10 to clinical category mapping, Z48 surgery aftercare codes map to the default clinical categories of “Return to Provider” or “Medical Management” even if a surgical procedure was indicated in J2100 of the MDS. Although Z48 codes are not very specific, CMS understands that aftercare of some major non-orthopedic surgeries is coded through Z48 codes. Therefore, CMS has finalized adding the surgical option of “May be Eligible for the Non- Orthopedic Surgery Category” to the following surgery aftercare codes: Z48.21, Z48.22, Z48.23, Z48.24, Z48.280, Z48,.288, Z48.298, Z48.811, Z48.812, Z48.813, Z48.815, and Z48.816, to promote more accurate clinical category assignment.
• With regard to the NTA comorbidity to ICD-10 code mappings, in the FY 2020 NTA comorbidity mapping, ICD-10 codes T82.310A through T85.89XA for initial encounter codes map to the NTA comorbidity CC176 “Complications of Specified Implanted Device or Graft”. This mapping only includes ICD-10 codes for acute encounters for complications of internal devices. It has been requested that CMS add to the mappings the ICD-10 codes in this range with the seventh digit of D (subsequent encounter) or S (sequela) for subsequent care. CMS has finalized adding codes in this range with the seventh digit of D (but not the seventh digit of S, because sequela can be coded years after the event and are likely not a reason for SNF treatment) for use in the ICD-10 code mapping to the NTA comorbidity CC176 “Complications of Specified Implanted Device or Graft” on the NTA conditions and extensive services list for the purpose of calculating the PDPM NTA score.
Finalized FY 2023 Value Based Purchasing measurements: Baseline FY 2019, Performance FY 2021
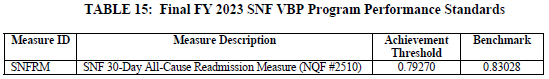
• CMS has finalized in prior rulemaking that they intend to use the Skilled Nursing Facility 30-Day Potentially Preventable Readmission Measure (SNFPPR) for the SNF VBP Program instead of the SNFRM as soon as practicable, as required by statute. CMS intends to submit the measure for NQF endorsement review during the Fall 2021 cycle, and to assess transition timing of the SNFPPR measure to the SNF VBP program after NQF endorsement review is complete.
• Considerations are being made regarding a separate reporting site for VBP data.
• TABLE 17 in the Final rule indicates SNF VBP Program Estimated Impacts for FY 2021.

