Henry David Thoreau once said, “Our least deed, like the young of the land crab, makes its way to the sea of cause and effect as soon as born, and makes a drop there to eternity.” This is true of the daily choices we all make in our personal lives. It is also true of the choices we make surrounding how much effort we put into understanding and applying the principles of the PDPM to our unique resident populations. In particular, the ripple effect that ICD-10 coding has on how CMS pays us for the care we provide to Part A beneficiaries.
At Broad River Rehab, we know how important accurate ICD-10 coding is to how a resident’s clinical characteristics are described within the PDPM grouper. Never before have ICD-10 diagnosis codes carried so much power over how a SNF will get paid for the kind of residents it cares for. Within the PDPM payment categories of Physical and Occupational Therapy (PT, OT), Speech Language Pathology (SLP), and Non-Therapy Ancillary Services (NTA), ICD-10 coding forms a foundation that can validate or devastate appropriate payment based on the resident’s unique clinical characteristics.
For FY 2022 there will be 72,747 ICD-10 codes in the PDPM clinical categories map, 102 in the SLP map and 2,117 in the NTA map for a total of 74,966 ICD-10 codes that have a potential impact on PDPM payment. The tables containing the FY 2022 codes can be found here. It is a daunting task to keep all of those codes and categories straight. It requires time and clinical prowess to apply them correctly to each resident’s unique clinical presentation.
Understanding the resident clinical presentation from an ICD-10 perspective is a critical skill when it comes to utilizing the PDPM accurately. CMS stated clearly in the lead up to the PDPM implementation that the new payment methodology was designed to help providers make better care decisions. Characterizing our residents with an accurate ICD-10 picture will go a long way to make CMS’ expectation a reality. We’ve created a way to make the process of using ICD-10 accurately within the PDPM grouper no nonsense.
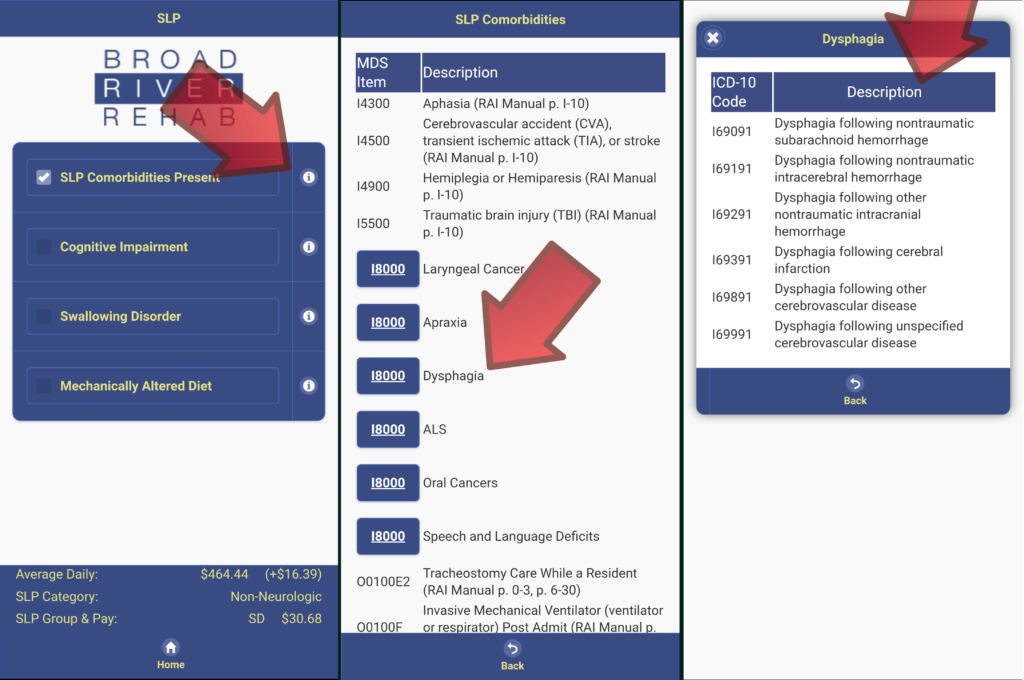
For example, in our PDPM Navigator® app, we have built in ICD-10 maps for each of the SLP and NTA comorbidities. This allows the user to see quickly what ICD-10 codes map to those particular categories. This handy, time saving tool allows the user to make fast ICD-10 decisions and creates a communication bridge to the IDT, in particular to the physician who can provide supporting documentation. The example below shows the SLP ICD-10 pathway. The NTA ICD-10 mapping pathway works the same way with the same result, fact effective accurate PDPM ICD-10 mapping. Consider how important accurate ICD-10 documentation is to the case mix splits in the NTA category, i.e., $30.56/day from E to D (ex. Urban base rates).
| Disease Category | Final Rule Rationale | FY 2022 Mapping Revision |
|---|---|---|
| Sickle Cell Disease | On October 1, 2020 two ICD-10 codes representing types of sickle-cell disease; D57.42 “Sickle-cell thalassemia beta zero without crisis” and D57.44 “Sickle-cell thalassemia beta plus without crisis” took effect and were clinically mapped to the category of “Medical Management”. However, there are more specific codes to indicate why a patient with sickle-cell disease would require SNF care, and if the patient is not in crisis, this most likely indicates that SNF care is not required. | For this reason, we will change the assignment of D57.42 and D57.44 to “Return to Provider”. |
| Esophageal Conditions | On October 1, 2020, three new ICD-10 codes representing types of esophageal conditions; K20.81 “Other esophagitis with bleeding”, K20.91, “Esophagitis, unspecified with bleeding, and K21.01 “Gastro-esophageal reflux disease with esophagitis, with bleeding” took effect and were clinically mapped to “Return to Provider”. Upon review of these codes, we recognize that these codes represent these esophageal conditions with more specificity than originally considered because of the bleeding that is part of the conditions and that they would more likely be found in SNF patients. | Therefore, we will change the assignment of K20.81, K20.91, and K21.01 to “Medical Management” in order to promote more accurate clinical category assignment. |
| Multisystem Inflammatory Syndrome | In December 2020, the CDC announced several additions to the ICD-10 Classification related to COVID-19 that became effective on January 1, 2021. One such code, M35.81 “Multisystem inflammatory syndrome”, was assigned to “Non-Surgical Orthopedic/Musculoskeletal”. However, Multisystem inflammatory syndrome can involve more than the musculoskeletal system. It can also involve the gastrointestinal tract, heart, central nervous system, and kidneys. | For this reason, we will change the assignment of M35.81 to “Medical Management” in order to promote more accurate clinical category assignment. |
| Neonatal Cerebral Infarction | On October 1, 2020, three new ICD-10 codes representing types of neonatal cerebral infarction were classified as “Return to Provider.” These codes were P91.821 “Neonatal cerebral infarction, right side of brain,” P91.822, “Neonatal cerebral infarction, left side of brain,” and P91.823, “Neonatal cerebral infarction, bilateral.” While a neonate is unlikely to be a Medicare beneficiary, this diagnosis could continue to be used later in life hence placing those with this condition in the acute neurologic category. | Therefore, we will change the assignment of P91.821, P91.822, and P91.823 to “Acute Neurologic” in order to promote more accurate clinical category assignment. |
| Vaping-Related Disorder | On April 1, 2020, U07.0, “Vaping-related disorder,” took effect and was classified as a “Return to Provider” code because at the time, “Vaping-related disorder” was not considered a code that would be a primary diagnosis during a SNF stay. However, upon further review, we believe that many patients who exhibit this diagnosis require steroids, empiric antibiotics and oxygen for care which could carry over to the post-acute setting. | For this reason, we will change the assignment of U07.0 to “Pulmonary” classification in order to promote more accurate clinical category assignment. |
| Anoxic Brain Damage | The ICD-10 code, G93.1 was initially clinically mapped to “Return to provider” because “Anoxic brain damage, not elsewhere classified” was non-specific and did not fully describe a patient’s deficits and may not have been an acute condition. However, upon further review, our clinicians determined that although this may not be an acute condition, “Anoxic brain damage, not elsewhere classified” would still likely result in a need for SNF care and is similar to conditions such as “Compression of the brain”, “Cerebral edema”, and “encephalopathy”, which are mapped into the “Acute Neurologic” category. | Therefore, we will change the assignment of G93.1 “Anoxic brain damage, not elsewhere classified” to “Acute Neurologic” |
Most of these are welcome changes and allow more flexibility for appropriate, accurate coding that will support care decisions from the reimbursement perspective. Accurate placement into the primary clinical category for the PDPM is an essential task that requires skill and a sharp capacity for critical thinking and clinical decision making. The primary diagnosis is a reflection of the primary medical condition category coded at MDS item I0020B and located at FL 67 on the UB-04. This diagnosis code is foundational to developing the case mix for the PT, OT and SLP payment categories. Missing this could have significant implications on your variable per diem rate.
Also, according to the RAI Manual, for the Primary DX: An ICD-10-CM code should be selected at MDS I0020B that, “…best describes the primary reason for the Medicare Part A stay.” And, CMS 100-2 Ch. 8 clarifies that, “To be covered the extended care services must have been for the treatment of a condition for which the beneficiary was receiving inpatient hospital services (including services of an emergency hospital) or a condition which arose while in the SNF for treatment of a condition for which the beneficiary was previously hospitalized. In this context, the applicable hospital condition need not have been the principal diagnosis that actually precipitated the beneficiary’s admission to the hospital, but could be any one of the conditions present during the qualifying hospital stay.” Filtering your ICD-10 choices through these instructions is also an important IDT skill.
Understanding and applying these guidelines along with the FY 2022 changes and where they apply in the PDPM grouper is complicated and often time consuming. Multiple documentation sources as well as perusing the ICD-10/PDPM maps is not rocket science, neither is it a simple 1+1=2 equation. In the examples below, notice that the PDPM Navigator® makes quick work of searching and finding appropriate ICD-10 primary diagnosis codes and clinical category placement.
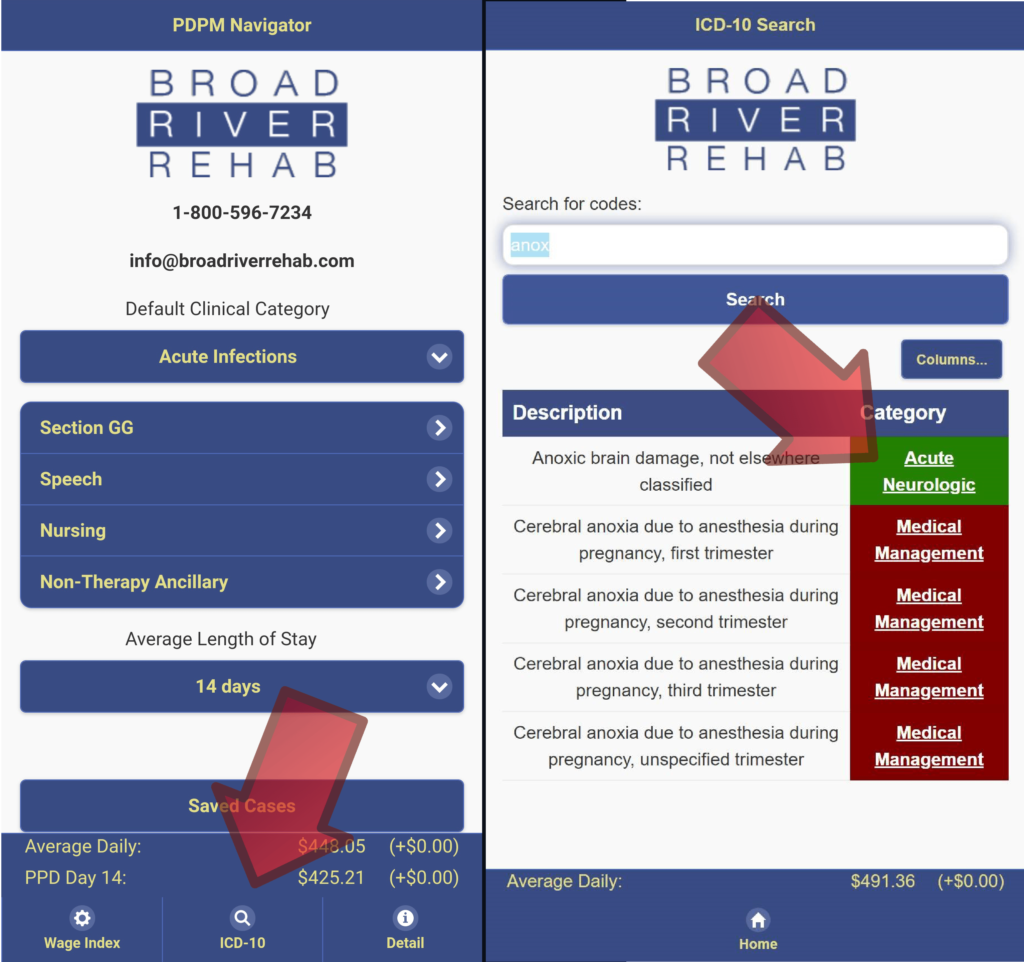
With tools like the PDPM Navigator® in hand providers in Buncombe Co. NC, for example, will quickly see the difference between selecting an ICD-10 code that would result in a primary diagnosis category of Medical Management (HIPPS JHNC average for 7 days – $593.30) vs. Acute neurologic (HIPPS NKNC average for 7 days – $616.99). In order for CMS’s expectation of better care decisions being realized out of the PDPM reimbursement system, being able to make these types of ICD-10 choices is a must. Broad River’s tools have been updated to the FY 2022 Final Rule changes and will be ready to meet these challenges on October 1.
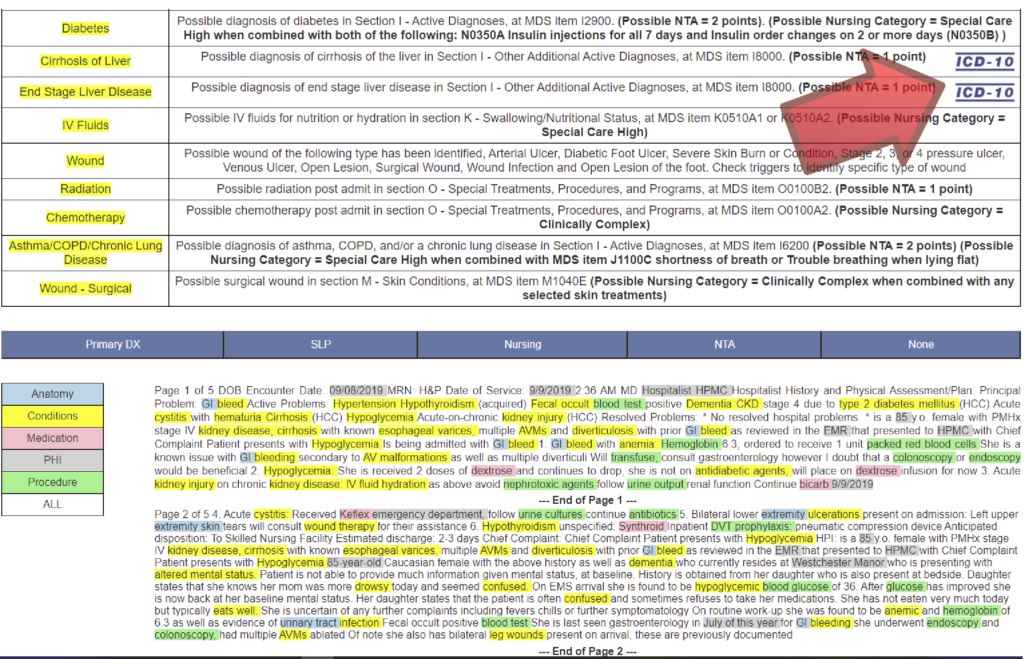
Wading through large stacks of admission documentation from the hospital while attempting to apply all of the PDPM ICD-10 requirements is no small accomplishment, in fact it’s impossible. There’s just too much to remember, too many tables and maps to consult. We also have a solution for this. Our Document Navigator™ combines the use of AI with practical visibility to help facility staff quickly identify the necessary items to consider relative to PDP. We often refer to these as the, “golden needles in the haystack.” Dragging and dropping a PDF into an AI tool is much simpler that trying to pick apart admission documentation by hand.
As you can see in the graphic below, the Document Navigator™ not only identifies items that need to be considered in light of PDPM, it also highlights the applicable ICD-10 maps and codes. One click, and the entire map of codes, relative to that NTA or SLP comorbidity, is available to view and discuss. This tool, combined with an embedded PDPM Navigator® allows fast, accurate clinical category ICD-10 decision making as well, that can result in accurate reimbursement for the care decisions that will need to be made for your residents.
It goes without saying that that Thoreau was right. Seemingly small and insignificant choices can have far reaching effects. This is no less true when it comes to PDPM ICD-10 coding decisions. It’s hard to believe that FY 2022 will be here in just a few short days. Will you be ready? Understanding and applying ICD-10 to PDPM will always be a necessary competency with lasting consequences. It’s time to drop that pebble into the pond and watch the ripples grow.

