Like a diamond, the new Patient Driven Payment Model (PDPM) is a multifaceted reimbursement system that reflects the various aspects of resident care in a SNF more clearly that the current RUG based system. It is a system that providers must master before it becomes the reality of how SNF’s are reimbursed beginning Oct. 1st. An important strategy that will enable providers to have success under this payment model will be to embrace a completely integrated approach in caring for their residents by partnering with vendors who understand how PDPM works and who will work as part of the care team to ensure that resident centered value and outcomes are achieved. This is especially true with regard to the Speech Language Pathology (SLP) category.
Under the current RUG system, often SLP has taken a back seat to other therapies. Also, in today’s RUG based world, SLP staff generally get involved only when a resident has been identified for whom a significant SLP related problem has already manifested itself. Often acute subtle neurological deficits go unnoticed that may be manifested first in the oral cavity, swallowing issues, communication and cognitive issues. For these there is often little or no chance for proactivity that may prevent or mitigate negative outcomes like weight loss, falls, behaviors and pain. While SLP involvement can be valuable at any stage of deficit development, early identification of SLP related deficits is key to determining appropriate treatment, achieving desired outcomes, and mitigating or even eliminating any negative consequences.
Another unfortunate reality in long term care is that many SLP related deficits often go unnoticed because they are routinely chalked up to “old age”. For example, a resident may cough routinely while eating, taking medications and at other times, and this may simply be disregarded as a consequence of a chronic illness such as COPD or chronic bronchitis. The same is true with communication deficits for individuals with progressive diseases like Alzheimer’s disease. These and other similar situations may be treated more appropriately with earlier SLP intervention.
Under PDPM, Speech Language Pathology (SLP) will finally be given it’s due in relationship to how important this vital service is. SLP must be multifaceted in its approach to resident care not only in how swallowing issues are identified and treated but in identifying and working with communication and cognitive deficit issues as well. With the advent of PDPM, savvy providers can take advantage of how the new system rewards innovative approaches to caring for populations that they may have overlooked or lately addressed in the past.
Here is how the SLP payment category works under PDPM. There are five SLP elements that must be routinely considered for each resident on Medicare Part A. They are:
-
The presence of an acute neurologic condition – This is determined by the primary ICD-10 CM diagnosis identified under the PT category and is either acute neurologic or not.
-
The presence of any SLP related Comorbidity – MDS items: I4300 Aphasia, I4500 CVA, TIA, Stroke, I4900 Hemiplegia, Hemiparesis, I5500 Traumatic Brain Injury, O0100E2 Tracheostomy care while a resident, O0100F2 Invasive Mechanical Ventilator while a resident, !8000 Laryngeal cancer, Apraxia, Dysphagia, ALS, Oral cancers, Speech and language deficits.
-
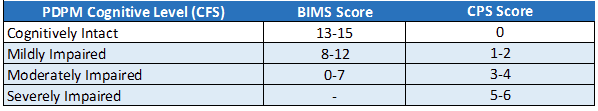
The presence of a mild to severe cognitive deficit – Determined by the new Cognitive Function Scale (see below)
-
The presence of a mechanically altered diet while a resident – coded at MDS item K0510C2
-
The presence of a swallowing disorder – coded at MDS items K0100A – K0100D
Once these elements are identified the table below is used to determine the actual SLP payment category. You will notice that missing any of the 5 SLP category determining elements could potentially have a negative effect of the resident centered care pathway but will also have significant impact on reimbursement.
For example, if a resident was assessed as having an acute neurologic condition and moderate cognitive impairment, they would fall into the SG category at $45.19/day for an Urban facility. However, suppose the facility failed to identify the comorbidity of dysphagia because the documentation from the hospital did not contain that diagnosis, and the resident routinely coughed, presumably from an identified chronic respiratory condition. Also, it has often been observed that the individuals responsible for evaluating items in section K of the MDS are dietary staff, many of whom have no special training related to identifying swallowing disorders or the need for a mechanically altered diet.
Misidentifying a diagnosis of Dysphagia, a swallowing disorder and the need for a mechanically altered diet would not only have negative consequences on resident care would also negatively affect reimbursement. Notice a difference of $47.62/day as the appropriate SLP category may very well be SL ($92.81) had the resident been assessed appropriately
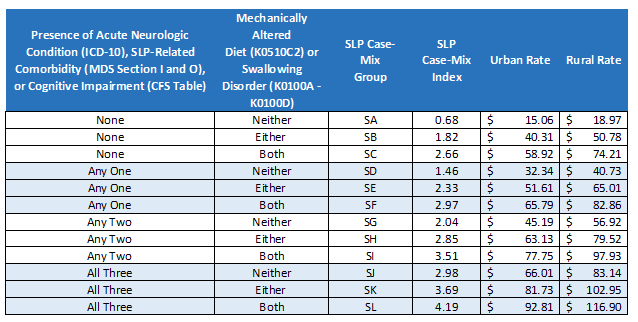
As you can see, understanding, appropriately evaluating and capturing the intricacies of all the SLP payment category elements is essential to providing appropriate resident care and obtaining equally
appropriate reimbursement. To that end, a completely integrated approach in caring for your residents by partnering with vendors who understand how PDPM works and who will work as part of a compassionate care team to ensure that resident centered value and outcomes are achieved is crucial.
At Broad River Rehab, we are uniquely situated to partner with SNFs as we approach PDPM. All our Regional VPs are AANAC RAC-CT certified and by Oct. 1, 2019, our goal is to have all our facility rehab directors RAC-CT certified as well. Two of our RVPs are highly qualified clinically competent Speech Language Pathologists. Broad River Rehab also employs MDS and reimbursement experts and our VP of Compliance and Regulatory Affairs 1 of only 34 AANAC Master Teachers in the U.S. We understand how PDPM works. We are ready to integrate our knowledge and compassion with your facility.
We would love for you to ask us PDPM related questions by clicking the “Ask an Expert” link. Or better yet, give us a call, we’d love to talk (800) 596-7234.
