Since the inception of the PDPM, providers have grappled with the nuances of the new payment system in an effort to ensure that reimbursement accommodate the services that are provided to each resident. The challenge has been that the PDPM is nothing like the former RUG-IV system in which facilities were essentially paid for volume of rehab services provided rather than on the merits of the unique health characteristics of the resident population they served.
With the shift away from volume as a basis for payment, the PDPM ushered in a new era of accountability inherent in the new payment construct which requires providers to make a legitimate analysis of the resident as a unique and individual person with a unique and personal health profile, rather than how many minutes and day of therapy they could perform.
Financial accountability is not a unique idea per se. Plenty of accountability networks exist, just ask the last victim of a TPE or RAC audit. Accountability within the framework of a payment system, however, is unique, and the PDPM has plenty of accountability built in. In the days leading up to the PDPM implementation, through the proposed and final rulemaking processes, CMS made the argument the new payment system was developed with a view to giving providers the ability to make better care decisions, ostensibly, through the appropriate use of the new payment construct.
We are all familiar with the fact that the PDPM consists of 5 payment categories, PT, OT, SLP Nursing and Non-Therapy Ancillaries. The final payment rate for each resident is to consists of how his or her unique clinical characteristics fit into those 5 categories. The unique accountability piece is that it is up to the facility staff to do due diligence to identify each these characteristics and capture them in the Minimum data set within the required timeframes in order to be reimbursed at the level CMS has determined to be appropriate based on that unique set of characteristics.
The ability to be paid based on appropriate capture of resident characteristics is why CMS indicated that the PDPM was a system that would help providers make better care decisions. The reality is that this is true from a payment standpoint as well as the residual care pathway development that ensues from a well examined clinical case. This has proven to be a God send with in the current COVID PHE. Some providers have proven to have adapted well to this new process while other continue to lag behind. Opportunity abounds and the positive aspects of accountability that go with it.
The primary diagnosis is one of the many focus points of this special resident profile that facilities are charged with developing. Selecting the appropriate diagnosis is one of the elements of the PDPM that has proved elusive to many providers. The primary diagnosis is coded at item I0020B in the MDS and there are several guidelines that CMS has provided to help with its selection. Here are few samples.
From the RAI Manual pp I-1 and I-2
Intent: The items in this section are intended to code diseases that have a direct relationship to the resident’s current functional status, cognitive status, mood or behavior status, medical treatments, nursing monitoring, or risk of death. One of the important functions of the MDS assessment is to generate an updated, accurate picture of the resident’s current health status.
Steps for Assessment:
-
I0020 – Indicate the resident’s primary medical condition category that best describes the primary reason for the Medicare Part A stay.
-
I0020B – Enter the International Classification of Diseases (ICD) code for that condition, including the decimal.
From the PDPM FAQ document
2.1 How will ICD-10 codes be used under PDPM?
There are two ways in which ICD-10 codes will be used under PDPM. First, providers will be required to report on the MDS the patient’s primary diagnosis for the SNF stay. Each primary diagnosis is mapped to one of ten PDPM clinical categories, representing groups of similar diagnosis codes, which is then used as part of the patient’s classification under the PT, OT, and SLP components. Second, ICD-10 codes are used to capture additional diagnoses and comorbidities that the patient has, which can factor into the SLP comorbidities that are part of classifying patients under the SLP component and the NTA comorbidity score that is used to classify patients under the NTA component.
1.7 Will providers still report the patient HIPPS code in the same way on the UB-04?
Yes, SNF billing practices related to the use of the HIPPS code and revenue codes remain the same under PDPM.
1.8 Is it required that the principal diagnosis on the SNF claim match the primary diagnosis coded in item I0020B?
While we expect that these diagnoses should match, there is no claims edit that will enforce such a requirement.
1.9 Is it required that the SNF primary diagnosis match the primary diagnosis reported for the qualifying hospital stay?
No, the primary diagnosis for the SNF stay may differ from the primary diagnosis reported for the hospital stay that serves as the qualifying hospital stay necessary for SNF coverage.
From CMS 100-2 Ch. 8
“To be covered the extended care services must have been for the treatment of a condition for which the beneficiary was receiving inpatient hospital services (including services of an emergency hospital) or a condition which arose while in the SNF for treatment of a condition for which the beneficiary was previously hospitalized. In this context, the applicable hospital condition need not have been the principal diagnosis that actually precipitated the beneficiary’s admission to the hospital but could be any one of the conditions present during the qualifying hospital stay.”
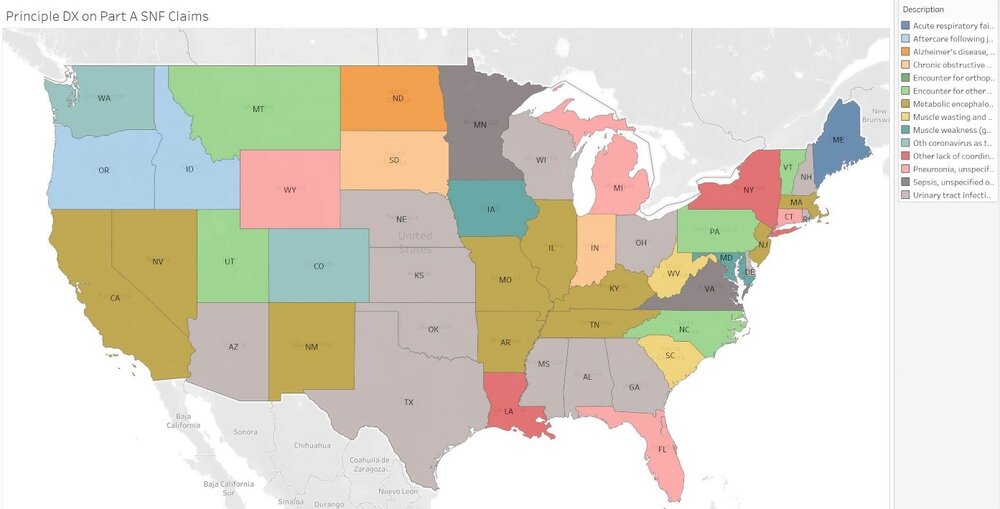
So much to consider. Yet the primary diagnosis, as one of many critical PDPM elements that help define the resident characteristic profile, acts as a foundation for the PT, OT and SLP categories. Getting it right not only sets the stage for proper reimbursement in these categories, but as many have discovered, it opens the door to a whole world of appropriate care decision making as well. Note the Nationwide distribution of most used SNF principal diagnosis codes used during Q2 2020 as well as the PT, OT and SLP payment categories below.
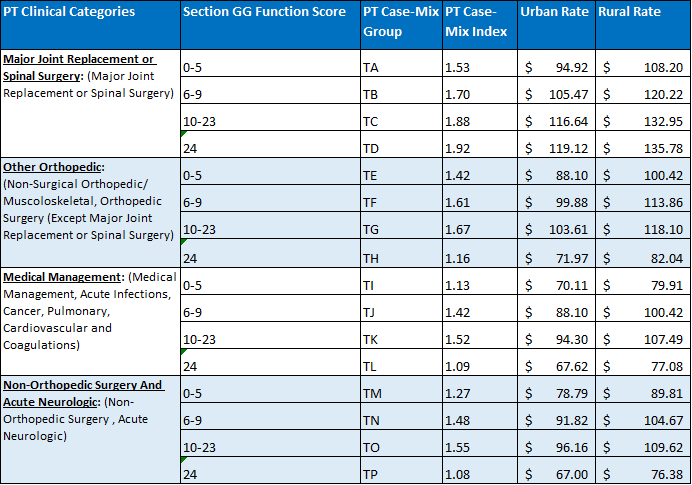
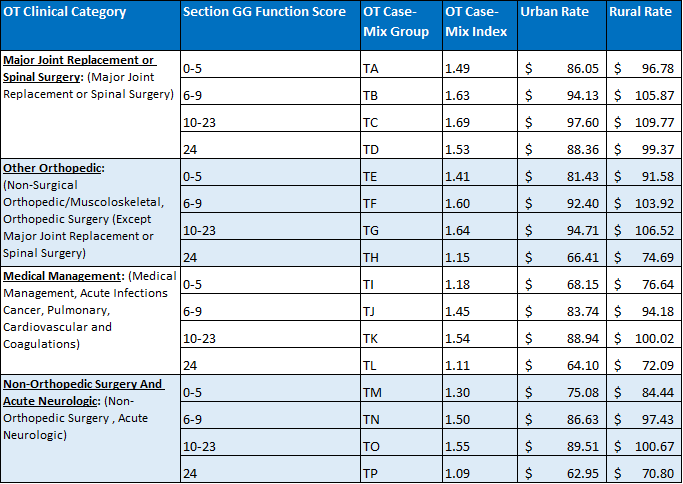
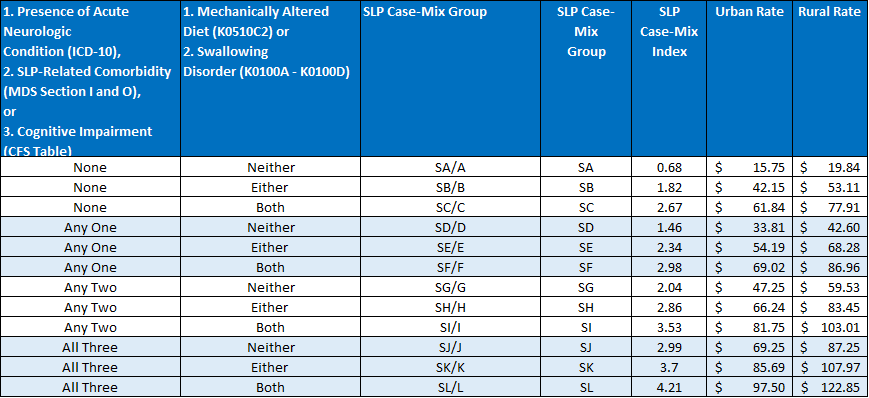
Each of these payment categories is first defined by placement into one of 4 unique diagnostic categories that has as its basis one of several thousand ICD-10 codes from the clinical category map the CMS has prepared. The RAI guidelines indicate that this one code is to best represent the primary reason for the resident’s skilled stay. It is a daunting task to select one unique code that does this special task. Yet that is the accountability built into this system.
If the provider has completed this task appropriately, not only will they begin the path toward receiving reimbursement that should compensate the unique care needs of the resident, they will have initiated a care decision process that will give the entire IDT a leg up as to a more holistic expression of the resident specific care delivery pathway.
I like to think of it this way from an example on page I-3 of the RAI Manual.
Example: Ms. K is a 67-year-old female with a history of Alzheimer’s dementia and diabetes who is admitted after a stroke. The diagnosis of stroke, as well as the history of Alzheimer’s dementia and diabetes, is documented in Ms. K’s history and physical by the admitting physician.
Coding: I0020 would be coded 01, Stroke. I0020B would be coded as I69.051 (Hemiplegia and hemiparesis following non-traumatic subarachnoid hemorrhage).
Rationale: The physician’s history and physical documents the diagnosis stroke as the reason for Ms. K’s admission. The ICD-10 code provided in I0020B above is only an example of an appropriate code for this condition category
In this example, the facility chose I69.051 Hemiplegia and hemiparesis following non-traumatic subarachnoid hemorrhage which maps to the Non-Orthopedic and Acute Neurologic clinical category. They just as well could have chosen another similar ICD-10 code that mapped to Medical Management. Note the guidelines indicate that the ICD-10 code provided in I0020B in the example is only an example of an appropriate code for this condition category. The wisdom in selecting I69.051 includes the knowledge that this code reflects a much broader range of clinical characteristic uniqueness, i.e. the neurologic condition designation in the SLP category, than perhaps another code. It also includes an understanding that the SNF primary diagnosis does not have to match the hospital principle diagnosis.
Understanding of the clinical uniqueness and breadth of one primary diagnosis over another is key in benefiting from the built-in accountability in the PDPM for payment that leads to better care delivery decisions. Consider the issues facing our industry during the COVID PHE. Many of the residents that are currently being treated and will be treated, have experienced COVID-19 and will have to contend with the ongoing and often chronic and systemic nature of the aftereffects. Consider this list of systems that have been shown to be affected chronically by COVID-19 (Pulmonary, Cardiac, Neurologic, Hematologic, Renal, Integumentary, Hepatic, Musculature, Metabolic) The pool of research continues to grow indicating future COVID-19 body system issues. The effective use of the primary diagnosis code will serve facilities well as they begin to see the chronic effects of COVID.
It is imperative that clinicians and IDTs understand the power of the PDPM primary diagnosis. A right handling of this foundational PDPM component will open the door to resident centered care decision making that CMS intended in the design of PDPM and will lead to payment that will undergird those decisions.

