In a recent post we detailed the new SNF QRP measure, Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalizations and provided a draft of the measure specifications for your review. We provided a link to the announcement where CMS has called for public comment on the measure. That comment period ends October 14th. We also prognosticated that this measure would be fast tracked and applied to the SNF QRP and Care Compare in relatively short order.
As it turns out, without much fanfare, CMS has quietly posted data relative to this QRP measure in your CASPER folder for 2018 and 20109. You should check it out. In your CASPER folder you will find a report titled, SNF HAI Confidential Dry Run Report.
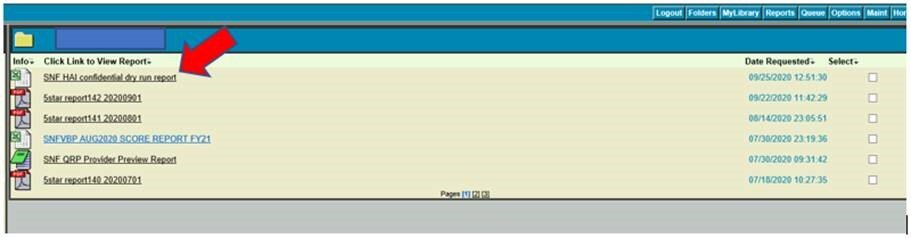
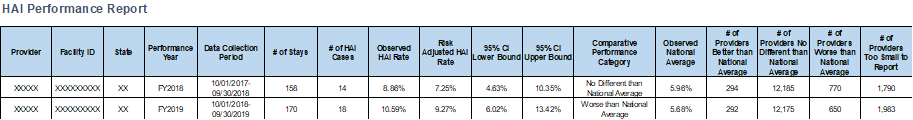
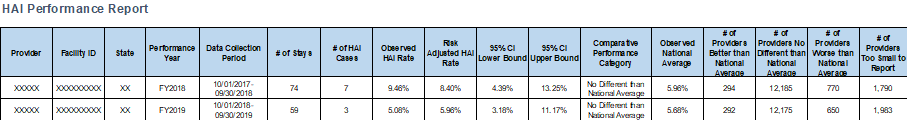
Here are a few examples of reports that will be found there. Just so you know what the data on these reports mean, the spreadsheet that you can download from CASPER includes a Descriptions tab that has measure and data details.
Briefly, here is what this measure measures and how it is calculated.
Healthcare associated infection (HAI) is defined as an infection acquired while receiving care at a health care facility that was not present or incubating at the time of admission. If the prevention and treatment of HAIs are poorly managed, they can cause poor health care outcomes for patients and lead to wasteful resource use. Most HAIs are considered potentially preventable because they are outcomes of care related to processes or structures of care. In other words, these infections typically result from inadequate management of patients following a medical intervention, such as surgery or device implantation, or poor adherence to hygiene protocol and antibiotic stewardship guidelines. Measuring HAIs among SNF residents can therefore provide valuable information about SNFs’ quality of care.
Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalizations measure will estimate the risk-standardized rate of HAIs that are acquired during SNF care and result in hospitalization. SNF HAIs that are acquired during SNF care and result in hospitalization will be identified using the principal diagnosis on the Medicare hospital claims for SNF residents, during the time window beginning on day four after SNF admission and within day three after SNF discharge.
The goal of this risk-adjusted measure is to identify SNFs that have notably higher rates of HAIs that are acquired during SNF care and result in hospitalization, when compared to their peers. The purpose of risk adjustment is to account for risk factor differences across SNFs, when comparing quality of care between them. In other words, risk adjustment “levels the playing field” and allows for fairer quality-of-care comparisons between SNFs by controlling for differences in resident case-mix.
The HAI definition includes conditions selected based on the following conceptual criteria:
• Infections that are likely to be acquired during SNF care and severe enough to require hospitalization (e.g., life-threatening methicillin-resistant Staphylococcus aureus infections)
• Infections related to invasive (not implanted) medical devices (e.g., infections associated with catheters, insulin pumps, and central lines; infection of tracheostomy stoma)
The HAI definition excludes infections that meet any of the following criteria:
• Chronic infections (e.g. chronic viral hepatitis B with or without delta-agent)
• Infections that typically require a long period of time to present (e.g. typhoid arthritis)
• Infections that are likely related to the prior hospital stay (e.g. postprocedural retroperitoneal abscess)
• Sequela and subsequent encounter codes (e.g. sequelae of inflammatory diseases of central nervous system)
• Codes that include “causing disease classified elsewhere” (e.g. meningitis in bacterial diseases classified elsewhere)
• Codes likely to represent secondary infection, where the primary infection would likely already be coded (e.g. viral endocarditis, pericarditis, myocarditis or cardiomyopathy)
• Infections likely to be community acquired (e.g. echinococcus granulosus infection of liver)
• Infections common in other countries and/or acquired through animal contact (e.g. subacute and chronic melioidosis)
• Pre-existing infections that fall within the Center for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN) Repeat Infection Timeframe (RIT) of 14 days.
Adjusted Numerator
The final numerator is a risk-adjusted estimate of the number of SNF stays predicted to have an HAI that is acquired during SNF care and results in hospitalization.
Adjusted Denominator
The measure denominator is the risk adjusted “expected” number of SNF stays with the measure outcome. The eligible stays for this measure are all Medicare FFS SNF stays that do not meet the exclusion criteria during the measurement period. SNF stays are excluded from the denominator if they meet one or more of the following criteria:
1. Resident is less than 18 years old.
2. The SNF length of stay was shorter than four days.
3. Residents who were not continuously enrolled in Part A FFS Medicare during the SNF stay, 12 months prior to the measure period, and 3 days after the end of SNF stay.
4. Residents who did not have a short-term acute care hospital stay within 30 days prior to the SNF admission date. The short-term stay must have positive payment and positive length of stay. 5.
5. Residents who were transferred to a federal hospital from the SNF. Rationale: Residents who are transferred to federal hospitals will have incomplete inpatient claims.
6. Residents who received care from a provider located outside of the United States, Puerto Rico, or a U.S. territory.
7. SNF stays in which data were missing or problematic on any variable used in the measure construction or risk adjustment. This also includes stays where Medicare did not pay for the stay.
There is much more that could be discussed about this measure. Risk adjustment methods and pre-existing condition criteria, for example, are both detailed in the draft measure, and are worth exploring. For the time being, you should download your SNF HAI Confidential Dry Run Report from CSAPER and determine how you are doing. ResDAC data indicates that there are a significant number of residents that are admitted to SNFs who are readmitted back to hospitals with septicemia and other types of infections. It’s time that facilities begin to get a handle on their own data relative to this issue. It’s likely that it won’t be long before your HAI data will be posted on NHC/Care Compare for all the world to see.

