Under PDPM, rehab will become a cost and no longer be a source of revenue. Since outcomes are still job one, you might be wondering just how you’re going to pay for the rehab that is necessary to achieve the best possible patient outcome.
Planning is critical to your success. Contrary to what a lot of people are saying you don’t have 11 months (as of today) to figure things out. If you see a website counting down to October 1st 2019 stay away. You need to start implementing your plan MUCH sooner than that. You can’t expect to have all of your program changes spin up on day one and work properly, right? Any good project manager will tell your to begin testing your systems and iterating through change cycles long before “go live” date.
Note: If you don’t yet have an implementation plan, contact us today and let one of our experts create a custom plan just for your situation. Since they’re AANAC RAC certified nurses, they understand the things you’re going to need including restorative and respiratory. Alternatively, you can ask your provider’s AANAC RAC certified experts.
But you can’t plan without knowing how much money you might have available when PDPM is fully implemented. While it’s impossible to know exactly because it depends on the underlying medical conditions of the patients arriving at your facility and many other factors like how effective you are at identifying opportunities, CMS did make an estimate based on 2017 data.
Your therapy provider should have already provided this data to you, discussed the implications and helped you formulate a plan, but in case yours didn’t and you don’t want to sift through that data yourself, allow Broad River Rehab to do it for you.
Note: Sorry mobile users, this next part works best on a large screen.
This map shows every provider in the United States and the CMS estimated change in PPD. Hover your mouse over the map to show the map controls. You can zoom in to see your specific facility. Hover your mouse over the facility dot to see the name of the facility, the change in PPD and the number of days utilized in 2017.
As you can see, there are trends by state, by provider type, by ownership, etc. There are also some underlying truths that Accumen discussed in the technical report. Significantly, if you are servicing a high number of ultra-high residents, you will likely see lower reimbursement.
We can take this a step further however and convert the PPD change to a percentage change:
Okay. Now that you’ve seen your facility and you have an idea how much your Medicare Part A reimbursement is going to change under PDPM, you probably have more questions. How exactly do you use this information? How do you compare to other facilities? How do I create an action plan that will have me ready for PDPM? etc. (hint: that last one is the one to be asking…)
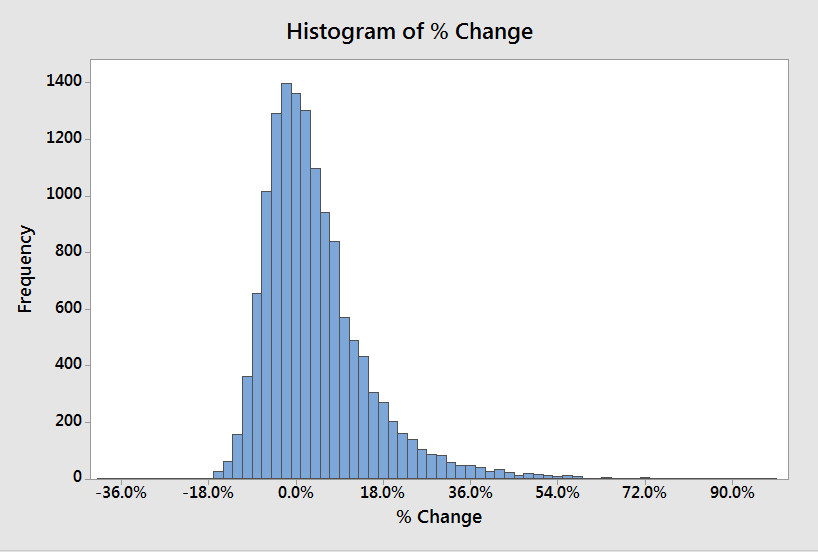
(click to enlarge)
Let’s start off with how you compare. The odds are the financial impact is positive. But, if you are one of the facilities that is expecting lower reimbursement, what should you do?
It might be tempting to just apply the same percentage decrease to your minutes but that’s not a sound strategy. Remember: your therapy contract is going to change with PDPM along with a LOT about the way your MDS nurse operates.
The best thing you can do at this point is educate yourself or at least find someone smart to talk it over with. Once you feel like you have a good understanding of how PDPM is going to work and how it will probably impact your facility, you need to engage your therapy contractor or therapy department. If your therapy partner is unwilling or unable to engage in serious, meaningful dialog about the operational and financial changes that will be required, it’s time to start finding outside help and considering change.
Not to put too fine a point on it, but… you know.

