I’m fortunate. I work for a forward-thinking company. We buy data from CMS and analyze it. We aggregate it. We look for trends. We study our own performance and look at how other people do it. We argue about what it means and how to get better at getting better. We have long debates about how to improve the lives of the people we serve, not just the people we treat. We even organize the data and give it away for free. Did you know that’s not free for us? We value knowledge, self-study and honest debate.
One trend we’re seeing that’s not in the data and is very concerning is the growth of Medicare Part A replacement plans. Well, it’s not the growth of the plans that’s necessarily the problem. The problem is the lack of accompanying data.
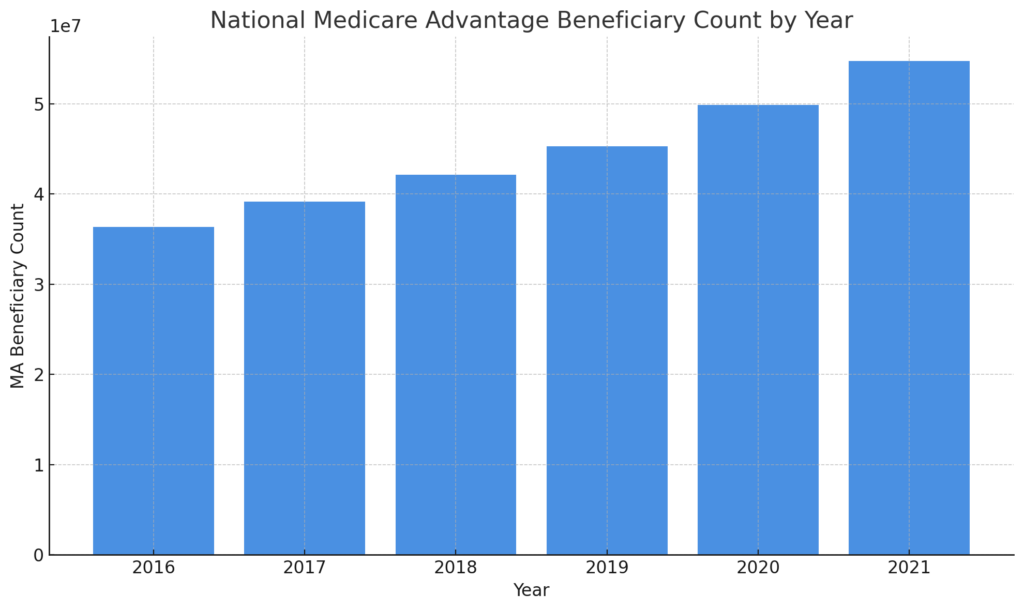
The Congressional Budget Office (CBO) has projected that Medicare Advantage share will reach 60% by the end of the decade1. Others project it will “only” reach 51% by that time2.
For the latest year we have published data, enrollment is approaching 70 million.
Yet, despite these programs being a “replacement” for Medicare Part A, none of the reporting we typically consume and analyze is available for these plans. In fact there is no meaningful reporting on Medicare Advantage plan performance in:
- Care Compare (formerly 5-star ratings)
- Quality Measures
- ResDAC
- data.cms.gov
About all we know is how many people are enrolled and how much it costs. Yet we can’t answer the most basic questions about those enrolled in Medicare Advantage plans:
- Are the people enrolled in these plans similar to those still enrolled in traditional Medicare Part A? Do healthier people somehow self-select or get recruited into these plans? Do they get similar outcomes?
- Do the people in these plans have similar length of stay numbers? Are they receiving similar services? Are they discharged to similar locations? Do they go to the hospital at similar rates?
- What are the denial rates? Is it similar to traditional Medicare Part A? Are denial rates rising?3 Do people get denied for Medicare Advantage Plans that would have been covered under traditional Medicare? If so, how are the plans a “replacement”?
Right now, all we have are rumors. This is no way to run a modern healthcare system. Data is the key to decision making. Skilled nursing providers are at a huge disadvantage without data.
Skilled nursing facilities have incredibly high burdens when it comes to submitting documentation. The “minimum” data set is more than 50 pages for each admission. Facilities endure audits, inspections, requests for additional information, “probes” and more. That’s just from CMS and doesn’t even include the hoops Medicare Advantage plans require. Why is it that Medicare Advantage plans don’t have to prove to us that what they do is working, at least as well as traditional Medicare?
So far, prior authorization has been the focus for reform. While that’s obviously important, it’s not nearly enough. The industry needs comprehensive and complete reporting that meets or exceeds what we currently see for Medicare Part A.

