Every day now we are hearing and reading about quality issues in the nursing home. The Pandemic has thrown a spotlight on areas that needed to be exposed. Focused infection control survey data now impacts your facility’s 5-star rating and new quality measures are constantly being introduced as measures under consideration or are being proposed for implemented. The current Value Based Purchasing rehospitalization incentive has also been scrutinized and impotent to cause change and is being reimagined.
The FY 2022 SNF PPS Proposed Rule has very much to say with regard to these issues. Significant updates to the SNF Quality Reporting Program (SNFQRP) and the SNF Value Based Purchasing Program (SNFVBP) are being proposed. This is a story has been lost in the discussion about wage index and rate updates and possible parity adjustment. But we should take a closer look at what CMS has proposed and intends related to quality measurement and value-based purchasing in FY 2022 and beyond.
First, we need to remember that the IMPACT Act from 2014 has set the stage for where we are headed regarding quality measurement in Post-Acute Care. The Improving Medicare Post-Acute Care Transformation Act (IMPACT) Act of 2014 requires the Secretary to implement specified clinical assessment domains using standardized (uniform) data elements to be nested within the assessment instruments currently required for submission by Long-Term Care Hospital (LTCH), Inpatient Rehabilitation Facility (IRF), Skilled Nursing Facility (SNF), and Home Health Agency (HHA) providers.
The Quality Reporting Program, or QRP, was the spawn of that legislation and we have been feeling the effects ever since. Currently there are 11 quality measures that have been developed for SNFs as a result with more to come, filtered through the meaningful measures framework, with an abundance of Standardized Patient Assessment Data Elements or SPADES to follow. Currently, the QRP measures 11 separate quality measures. Eight derive from the Minimum Data Set and three from Medicare claims. Only two of these measures, noted below, currently affect a facility’s 5-star rating. Here is the current list.
MDS Based
- Application of Percent of Residents Experiencing One or More Falls with Major Injury
- Application of Percent of Long-Term Care Hospital (LTCH) Patients with an Admission and Discharge Functional Assessment and a Care Plan that Addresses Function
- Drug Regimen Review Conducted with Follow-Up for Identified Issue
- Changes in Skin Integrity Post-Acute Care: Pressure Ulcer/Injury (5-Star)
- SNF Functional Outcome Measure: Change in Self-Care Score for Skilled Nursing Facility Residents
- SNF Functional Outcome Measure: Change in Mobility Score for Skilled Nursing Facility Residents
- SNF Functional Outcome Measure: Discharge Self-Care Score for Skilled Nursing Facility Residents
- SNF Functional Outcome Measure: Discharge Mobility Score for Skilled Nursing Facility Residents
Claims Based
- Medicare Spending Per Beneficiary – Post-Acute Care
- Discharge to Community (5-star)
- Potentially Preventable 30-Day Post-Discharge Readmission Measure
The FY 2021 Proposed and final Rules indicated the addition of two more MDS based measures along with multiple Standardized Patient Assessment Data Elements, or SPADES, that will be added after the Pandemic, all of which will require new MDS items. MDS 3.0 v1.18.0 which contained these additional elements, slated to be effective October 2020, was withdrawn due to pandemic related issues, and other concerns. Here is a list of the impending items.
- Transfer of Health Information to the Provider–Post-Acute Care (PAC);
- Transfer of Health Information to the Patient–Post-Acute Care (PAC).
- 3 SPADEs for Cognitive Function.
- 15 SPADEs to Assess for Special Services, Treatments, and Interventions.
- 1 SPADE to Assess for Medical Conditions and Co-Morbidities.
- 2 SPADEs to Assess for Impairments
- 5 SPADEs to assess for a new category: Social Determinants of Health.
The FY 2022 Proposed rule adds two more measures to the SF QRP which are proposed to be implemented starting October 2021.
- Claims Based: Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalizations Measure for the Skilled Nursing Facility Quality Reporting Program.
- NHSN Reporting: COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) Measure
All of the SNF QRP measures, except for the claims-based measures affect a SNFs annual APU or Annual Payment Update. If 100% of the data necessary to calculate the measure is not available on 80% of the MDS assessments completed, the facility will receive an annual 2% reduction to the market basket adjustment for that that FY. CMS has indicated that the vaccination measure will affect the APU but have yet to detail how.
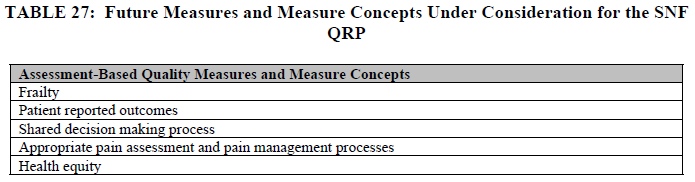
Finally, CMS is always considering new measures to implement. In the FY 2022 Proposed Rule they have posted the following Measures Under Consideration List.
Second, it is important to remember that CMS sees quality as a vital measure of how providers should be paid and so rehospitalizations, or Value Based Purchasing (VBP) has been the measure that has had the most impact on a SNF’s annual PPS rate since the measure was implemented as a result of PAMA, or the Protecting Access to Medicare Act, also from 2014.
The current measure that is utilized for this purpose is NQF 2510, Skilled Nursing Facility 30-Day All-Cause Readmission Measure or SNFRM. The SNFRM estimates the risk-standardized rate of all-cause, unplanned hospital readmissions for SNF Medicare fee-for-service (FFS) beneficiaries within 30 days of discharge from a prior proximal acute hospitalization.
Each FY, CMS withholds 2% of SNF payment and the individual facility performance compared to all other facilitates in the nation determines how much of that 2% the facility will earn back as a VBP incentive payment. Individual facilities receive quarterly confidential feedback reports in CASPER and an annual update related to that year’s incentive payment.
In the proposed rule, CMS has indicated that it is not their intention to penalize SNFs based on measure scores that they believe are distorted by the COVID-19 pandemic and are thus not reflective of the quality of care that the measure in the SNF VBP Program was designed to assess.
CMS is proposing to adopt a policy for the duration of the PHE for COVID-19 that would enable suppressing the use of SNF readmission measure data for purposes of scoring and payment adjustments in the SNF VBP Program if it is determined that circumstances caused by the PHE for COVID-19 have affected the measure and the resulting performance scores significantly.
Under this proposed policy, if CMS determines that the suppression of the SNF readmission measure is warranted for a SNF VBP program year, they will propose to calculate the SNF readmission measure rates for that program year but then suppress the use of those rates to generate performance scores, rank SNFs, and generate value-based incentive payment percentages based on those performance scores
CMS would instead assign each eligible SNF’s performance score of zero for the program year to mitigate the effect that the distorted measure results would otherwise have on SNF’s performance scores and incentive payment multipliers.
They would also reduce each eligible SNF’s adjusted Federal per diem rate by the applicable percent (2 percent) and then further adjust the resulting amounts by a value-based incentive payment amount equal to 60 percent of the total 2% reduction resulting in a 1.2 percent payback for the FY 2022 program year. CMS sees this as the most equitable way to reduce the impact of the withhold in light of the proposal to award a performance score of zero to all SNFs.
Those SNFs subject to the Low-Volume Adjustment policy would receive 100 percent of their 2 percent withhold per the policy previously finalized in the FY 2020 SNF PPS final rule.
CMS would also provide each SNF with its SNF readmission measure rate in confidential feedback reports so that the SNF is aware of the observed changes to its measure rates. CMS would also publicly report the FY 2022 SNF readmission measure rates with appropriate caveats noting the limitations of the data due to the PHE for COVID-19.
Finally, CMS has proposed steps to eliminate the effect of the covid pandemic on future measurement periods and VBP incentives by eliminating the heaviest COVID related time periods from those parameters.
Importantly, this past year, there have also been voices raised from various quarters related to the “ineffectiveness” of the current VBP measure related to its impact on facility behavior. It its March 2021 report, the Medicare Payment Advisory Committee or Medpac, made the following observations.
“In September 2020, the Commission discussed several shortcomings of the program’s design; in October 2020, it considered an alternative design that corrects them. Those discussions highlighted the lack of claims-based quality measures and a measure of patient experience for all PAC providers, including SNFs. Regarding the incentives established by the program, the trade press has noted that the size of the program’s payments may be too small to change behavior.”
In the FY 2020 proposed rule, CMS has taken up this mantle and has continued the discussion about just what those additional measures might look like. On December 27, 2020, Congress enacted the Consolidated Appropriations Act, 2021 part of which contains amendments to, with respect to payments for services furnished on or after October 1, 2023, require the Secretary to apply the specified readmission measure and allow the Secretary to apply up to 9 additional measures determined appropriate.
In the proposed rule, CMS sought input from stakeholders regarding which measures should be considered to be added to the SNF VBP Program. CMS intends to use future rulemaking to address these new statutory requirements.
In the meantime, the SNF VBP Program includes only a single quality measure, the SNFRM, which CMS intends to transition to the Skilled Nursing Facility Potentially Preventable Readmission measure SNFPPR measure as soon as practicable.
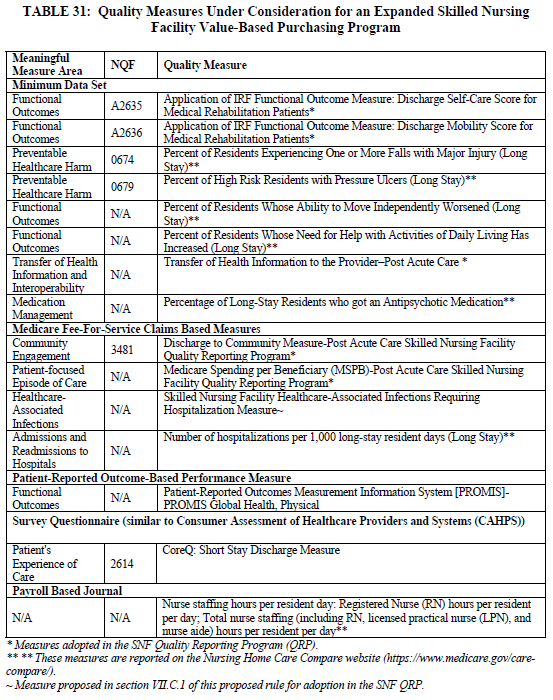
In considering which measures might be appropriate to add to the SNF VBP Program, CMS is considering additional clinical topics such as measures of functional status, patient safety, care coordination, and patient experience, as well as measures on those topics that are utilized in the SNF Quality Reporting Program (QRP).
CMS is also considering measures on clinical topics that are not included in the SNF QRP’s measure set because they believe that other clinical topics would be helpful to our efforts to robustly assess the quality of care furnished by SNFs.
In expanding the SNF VBP measure set, CMS is also considering measures that are already required for Long-Term Care Facilities (LTCFs), which include both SNFs and nursing facilities (NFs), to collect and report under other initiatives.
The vast majority of LTCF residents are also Medicare beneficiaries, regardless of whether they are in a Medicare Part A SNF stay. Therefore, CMS believes that expanding the SNF VBP measure set to assess the quality of care that SNFs provide to all residents of the facility, regardless of payer, would best represent the quality of care provided to all Medicare beneficiaries in the facility. Table 31 below include measures that CMS could add to the SNF VBP Program measure set.
In addition to the staffing measures listed in Table 31 that focus on nurse staffing hours per resident day and that are currently reported on the Nursing Home Care Compare website, CMS is also interested in measures that focus on staff turnover. CMS has been developing measures of staff turnover with the goal of making the information publicly available. CMS has indicated that they will be reporting rates of turnover in the future.
There are teeth in the FY 2022 SNF PPS proposed rule, beyond the payment updates and parity adjustment proposals that have garnered most of the spotlight in this year’s discussions. However, providers will be well served to be aware of the trajectory that CMS has proposed with regard to quality measurement and Value Based Purchasing in this year’s rule. The new normal post COVID is quality. Take that to the bank… or not.

